Progressive multifocal leukoencephalopathy is a viral disease that affects immunosuppressed patients. Therefore, it has been regularly associated with AIDS.
Progressive multifocal leukoencephalopathy is a rare and fatal viral disease in which the white matter of the brain is damaged and inflamed at multiple sites. It is caused by the John Cunningham virus (JC virus) and affects 4-8% of AIDS patients.
This pathology is exclusive to people with a weakened immune system, as the JC virus is controlled by circulating cells that defend the body from pathogens. The mortality rate in the immunosuppressed in the first months after infection is 50%.
What causes progressive multifocal leukoencephalopathy?
The etiologic agent of progressive multifocal leukoencephalopathy (PML) is the JC virus, a very common polyomavirus in the general population that usually causes asymptomatic infections during childhood.
This is a microscopic agent 45 nanometers in diameter, composed of double-stranded DNA of 5 to 13 kilobases (5,000 to 13,000 nucleotide pairs), wrapped in a capsid without an accessory lipoprotein layer. As the journal Neurological Disorders indicates, the virus is cosmopolitan and its best-known route of transmission is the fecal-oral route.
Half of the infections occur from children to parents within the home. This virus affects 70-90% of the world’s population at some point in their life and almost all people have already contracted it before the age of 40. As we have said, it generates asymptomatic infections, but the picture is different in immunosuppressed patients.
Pathogenic mechanism of the virus
Once the virus enters the human body, it usually settles in the palatine tonsils, accumulations of lymphoid tissue at the bottom of the oral cavity, on each side of the throat. After that, it travels to the gastrointestinal tract and settles in the mucous cells of the intestine or kidneys, remaining inactive and latent.
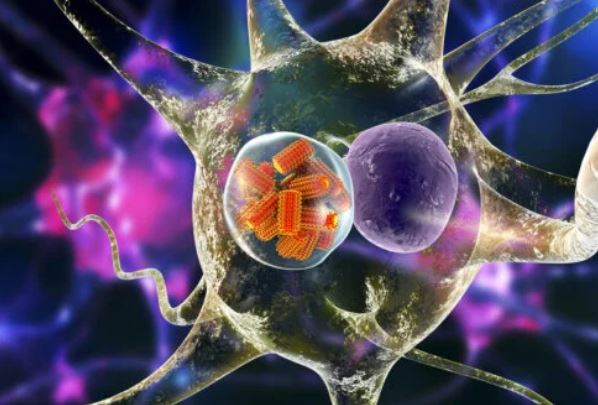
It should be noted that the genetic disposition of the JC virus is different in its active and inactive forms, as indicated by the StatPearls portal. When the pathogen goes from dormant to infective, it can invade brain tissue, resulting in the destruction of the myelin sheaths of neurons.
Myelin sheaths are the lining of neuronal axons. They allow the transmission of nerve impulses over relatively long distances, since they isolate the neuron from the environment. Once this protective layer has been damaged, the virus enters the nucleus of the oligodendrocytes and causes even more damage.
All this also causes infiltration of lymphocytes and inflammatory responses in the affected area. Ultimately, the white matter of the brain is irreversibly damaged.

Neurons are attacked by the JC virus on their myelin sheath, resulting in nerve conduction disorders.
Progressive multifocal leukoencephalopathy and HIV
In the first instance, it is necessary to emphasize that HIV and AIDS are not the same. An HIV-infected patient presents an acute symptomatic initial stage, but then the pathogen acts slowly and continuously. The human immunodeficiency virus, little by little, enters the CD4 lymphocytes and destroys them.
According to the HIV Info portal, a patient infected with HIV passes to the stage of AIDS when the CD4 lymphocyte count is less than 200 per cubic millimeter of blood. This means that your immune system has lost part of its functionality and therefore harmless pathogens can become a real problem.
The JC virus takes advantage of this immunosuppression to cause the aforementioned picture. For this reason, 80% of patients with progressive multifocal leukoencephalopathy are HIV positive and in the late stage of the disease (AIDS). The prognosis 2 years after the onset of symptoms is very poor.
Other risk factors for PML
Beyond AIDS, hematological malignancies are the cause of 10% of cases of progressive multifocal leukoencephalopathy (PML). Cancer of the leukemia or Hodgkin lymphoma type can affect the number of circulating viable lymphocytes, which is expressed as immunosuppression.
On the other hand, 5% of PMLs are caused by the consumption of the drug natalizumab, prescribed in the treatment of multiple sclerosis, psoriasis and lupus. Monoclonal antibody therapy has been associated with the onset of the disease, although much remains to be learned.
Symptoms and development of the disease
As indicated in the MSD Manuals, the virus remains dormant and does not cause symptoms until it is reactivated. There is some controversy, as some researchers have detected the JC virus within the brain tissue of healthy patients, while others argue that it only invades this area at the time of aggressive infection.
Be that as it may, the general symptoms depend on the area of the brain that is attacked first. Among the most common clinical signs we can mention the following:
Clumsiness, weakness, and difficulty speaking and thinking. Motor deficit, cognitive impairment and visual problems are the 3 pillars of demyelinating diseases.
As the disease progresses, the patient has severe difficulty moving and fending for himself. Limb weakness dramatically worsens over time.
In general, in a few months the patient will be bedridden. It is normal for death to occur between 1 and 9 months after the onset of symptoms. Above all, the disease reports an extremely poor prognosis in people with blood cancers.
The onset can be gradual, slow or subacute. The greater the immunocompromise of the patient, the faster and more aggressive the demyelination process will occur. In any case, more than half of the patients die irretrievably.
Diagnostic tests
According to the US National Library of Medicine, looking at a patient’s history is the first step in detecting progressive multifocal leukoencephalopathy. Once the pathology derived from immunosuppression is suspected, many diagnostic tests can be used; among them the blood test with leukocyte count.
If the patient has less than 200 CD4 lymphocytes for each cubic millimeter of blood, it is linked to HIV and AIDS. This, along with a blood PCR, can help determine the presence of circulating human immunodeficiency virus in the stream of the sick person.
Once superficial tests have been performed, imaging techniques (such as computed tomography or nuclear magnetic resonance) are used. This can help to show the damage and inflammation in the neuronal tissue, as well as the foci of affectation in the brain.
Finally, a cerebrospinal fluid test to look for the JC virus can be done as a final diagnostic step. In rare cases, a brain tissue biopsy is also used, although it is not usually necessary.

Brain biopsy is a resource that is not widely used for this diagnosis, since it does not add more value to therapy.
Treatment of progressive multifocal leukoencephalopathy
As we are facing a viral disease, the use of antibiotics is useless. The possible effect of many antiviral drugs (such as cidofovir) in this condition has been explored, but the results are not conclusive. Other drugs to treat certain cancers have also been tried, but they don’t seem to work.
For this reason, the main approach is based on autoimmune restoration, as indicated by the Elsevier portal. In AIDS patients, antiretroviral therapy (ART) is very useful, since it increases the CD4 lymphocyte count considerably and decreases the prevalence of the JC virus in the cerebrospinal fluid.
However, even though the leukocyte count improves, the neurogenic damage remains over time. For this reason, patients who survive are usually left with permanent sequelae in terms of psychomotor skills, cognitive development and vision. It is difficult for this pathology to come to fruition.
Serious prognosis in all its variants
As you have seen, we are facing an aggressive disease, of rapid onset, with obvious symptoms and a fatal prognosis. The virus that causes progressive multifocal leukoencephalopathy is not the problem by itself, since what is serious is the patient’s condition prior to infection and its inability to generate an immune response.
Unfortunately, it is impossible to end on a positive note. In the case of HIV-positive patients, their lives can be saved, but the long-term prognosis has not yet been elucidated. In the setting of people with leukemia or lymphomas, the survival rate approaches 0%.
In any case, it should be noted that only a small percentage of those infected with AIDS end up developing this pathology. Furthermore, with antiretroviral therapies (ART), a patient with HIV can lead a normal life; even without getting AIDS at any time.





